-
Improving Transitions of Care for Newborns Requiring Home Phototherapy Through Innovation & Collaboration
Carla Bieniek and Kristi Patterson
Improve transitions of care for newborns requiring home phototherapy by providing skilled nursing services through Home Care and changing the phototherapy modality from the BiliBed to the BiliSoft which provides more intense home phototherapy & is easier to administer.
-

Heart Huddle: Increasing Cohesiveness in CCU and CVTU
Ashley Douvier
The American Association of Critical Care Nurses identifies six standards for a healthy work environment, two of which are skilled communication and true collaboration. CCU and CVTU are two separate units staffed by one Charge RN. A need to improve communication and collaboration has existed throughout both units. Thus, Heart Huddle has been developed. The objective of Heart Huddle is to bring cohesiveness to CCU and CVTU through improving communication and collaboration, which is imperative to a healthy work environment.
-

Reduction of Cesarean Section Surgical Site Infections (SSI): Progression and Implementation of Evidence Based Practice
Patricia Dumonceaux, Melissa Erickson, Kim Schuster, and Elizabeth Kiffmeyer
To improve cesarean section patient experience by reduction of postoperative SSI.
-

Inpatient Rehabilitation Performance Improvement: Skin Care and Guidelines
Golden Fisk
To improve skin integrity care as well as use of hospital policies and guidelines within Inpatient Rehabilitation.
-

Best Practice for Core Charge Nurse Orientation and Leadership Development
Melissa Fradette
Purpose Statement: Develop and implement evidence based, standardized orientation and leadership development for core charge nurses (CCN) compared to current unit-based orientation which has inconsistent content and structure.
-
ETC Code Stroke Improvement
Melissa Fradette and Jessica Miller
There was a 42% increase in median times for patients receiving alteplase (tPA) within 60 minutes from 48 minutes in Q3FY13 to 68 minutes in Q1FY15. Research indicates every 15 minute delay in stroke treatment, the odds of good outcome decreased by 10%. During two day rapid improvement event team members and content experts used process mapping to identify waste in current state ETC Code Stroke process and determine countermeasures to eliminate waste and improve throughout.
-

Finding the Missing Pieces: Comprehensive Cerebellar Assessments with Cytarabine Administration
Tara Hinnenkamp
A study conducted at the University of Maryland Greenebaum Cancer Center found that one in four nurses felt there were widespread inconsistencies with cerebellar assessments. One of every two nurses felt the current assessment was incomplete and the patient may be suffering as a result. Nurses need to have the means to accurately and consistently assess and document neurological changes noted with Cytarabine administration.
-

Improving Bedside ECG Monitoring in Telemetry
Teresa Jahn, Jennifer Lang, and Jaclyn Hoppe
To improve accuracy of bedside ECG (EASI lead) monitoring through accurate placement of electrodes and proper skin preparation.
-

Reducing Overnight Vital Signs
Jill Libbesmeier
As delirium has been identified to increase functional decline, cost per patient day of hospitalization, and length of stay, previous delirium work has been completed at St. Cloud Hospital. Changes in sleep pattern and sleep environment have been identified as a cause of delirium. The purpose of this project is to change frequency of vital signs on Med 1, Med 2, and Medical and Oncology, allowing for increased uninterrupted periods of sleep to help reduce delirium rates; in turn reducing average length and cost of stay.
-

National Database of Nursing Quality Indicators
May Schomer
National Database of Nursing Quality Indicators (NDNQI) was launched by American Nursing Association (ANA) in 1998, with an initial set of ten quality indicators that assessed the quality of patient care. The continued mission of the NDNQI's is to improve patient care and safety by providing evidence based national research to nurses by comparing nursing care data and the connection this data has on patient outcomes. A relationship between patient outcomes and nurse staffing practices was noted, but further data collection was needed to appraise the quality of nursing care on each hospital unit in order to assess, evaluate and improve patient care outcomes. Unit level of care measurements empowers the nursing units to enhance their quality of patient care. To improve the quality of patient care, evidence-based practices are researched, developed, trialed, and implemented where needed.
-
Optimal Perioperative Management of the Geriatric Patient
Sherry Sonsalla
Purpose: Review best practice guidelines, perform a gap analysis, and provide recommendations for areas of opportunity for geriatric surgical patients.
-

Integrative Therapy Program: Evaluation and implementation of aromatherapy in an inpatient setting
Wendy Wheeler
Purpose Statement: The purpose of this project is to implement integrative therapies, such as aromatherapy, in addition to current nursing interventions. Goal is to improve patient experience and outcomes and enhance the patient/nurse relationship.
-

Opening an Observation Unit
Emily Zempel
The definition, benefits, and structure of an observation unit within a hospital.
-

Utilizing a Protocol to Reduce Post-Operative Urinary Retention in Total Joint Arthroplasty
Gina Anderson-Malum and Naomi Schneider
Foley catheters have not routinely been used for our total joint patients for many years, leading staff to bladder scan and straight catheterize patients postoperatively. Bladder scanning and catheterization were identified as an inconsistent practice. Patients were commonly straight catheterized when nurses determind bladder scan volume and time of last void; yet the amounts for both and decision to catheterize were inconsistent. Also, the clinical evaluation and treatment was inconsistent among physicians. Variations in practice included rationale for a urology consult, use of medications for urinary retention, and documentation. Baseline urinary retention condition codes ranged from 8-18%, which led our team to choose urinary retention as a performance meansure in 2012 for The Joint Commission Disease Specific Care Certification. Objective: Describe the clinical and cultural impact the total joint urinary protocol has on decreasing urinary retention.
-
Inpatient Rehabilitation Unit Specific Orientation
Joyce Belanger and Becky Kastanek
CMS has specific requirements for all Inpatient Rehab Facilities. Data collection in the form of FIM "Functional Independence Measure" is one of them. Due to these requirements, it was felt that we needed to provide further education to our new hire staff from all disciplines.
-
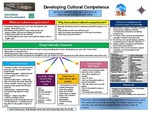
Developing Cultural Competence
Patricia Blonigen-Heinen and Roberta Basol
Caring for patients from many cultures is an important part of health care today. Why learn about cultural competencies? Because developing cultural competencies benefits everyone. You can: help patients receive more effective care; help your facility meet standards of The Joint Commission; and improve your job performance.
-

Sustaining Pressure Ulcer Prevention: Implementing a Skin Champion Model
Jennifer Burris
Purpose Question: Will an evidence-based skin champion model in the ICU improve nursing knowledge and perceptions about pressure ulcer prevention and reduce hospital acquired pressure ulcers?
-

Treating Early Sepsis Outside of the ICU Using a Bundle of Interventions
Jennifer Burris
To decrease cost and length of stay for sepsis patients by standardizing treatment in the progressive care units (PCUs).
-

Pneumonia: Ongoing Efforts to Improve Outcomes
CentraCare Health
Background: Original improvement efforts emphasized correct antibiotic, early mobilization, adequate hydration, and early and ongoing oxygen weaning. Ongoing efforts include: early mobilization, obtaining room air sats on admission, early and ongoing oxygen weaning, and patient education.
-

What the Heck is Value-Based Purchasing??
CentraCare Health
Medicare has changed the way hospitals get paid. The new payment program is called Value-Based Payments (VBP). VBP is made up of two parts: incentives & penalities.
-

Cultural Competency at the Bedside: Developing a Plan of Care for Limited English Proficiency Patient Populations
Jenna Czech
To improve nursing skills and competency in caring for culturally diverse and limited English proficiency patient populations.
-

Improving SCIP-4 Glucose Measures
Melissa Fradette
A performance improvement project was initiated to increase the Surgical Care Improvement Project (SCIP) glucose measure compliance. Order sets were modified to standardize glucose monitoring frequency and initiate insulin infusions. A previous practice of double documentation (manual and glucose meter interface documentation) were abstracted as 2 separate results. When glucose interfacting became an option, the practice of manual entries did not stop. The use of manually documented results for decisions failue to prompt interface confirmation; non-validated results do not interface. The plan: implement order set changes; eliminate manual documentation; and rely on interfaced measures to make clinical decisions.
-

Giving Time Back: Implementing a Electronic Nursing Protocol for Skin Care
Amy Gorecki, Sue Omann, and Kim Schuster
Purpose Statement: To improve the accessibility of evidence based skin care interventions for the clinical nurse without the need of a CWOCN consult.
-

Shifting the Paradigm of Classroom Nursing Orientation
Mary Leyk
Purpose Statement: The purpose of the Evidence-Based Practice Nursing Orientation Project is to find evidence to support a change in teaching strategy for newly hired RNs (both New Grads as well as experienced nurses), from the current process in order to improve outcomes of clinical competence, independence and nurse confidence, and retention.
-
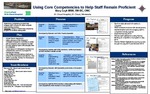
Using Core Competencies to Help Staff Remain Proficient
Mary Leyk
Problem: Implement a competency program that engages staff compared to usual computer-based training modules. Objective: Design a multi-modal competency program for bedside nursing staff.
Nurses at CentraCare Health are engaged in finding ways to improve all aspects of practice of nursing in the clinical setting. The following are posters created in the process of Evidence-based Practice Projects and clinical improvement.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.

